
Have you ever heard of keratoconus?
If not, you are not alone. Keratoconus is a relatively rare eye condition that affects about 1 in 2,000 people. Keratoconus, derived from the Greek words “kerato” meaning cornea and “konos” meaning cone. It can cause blurry and distorted vision, sensitivity to light, and frequent changes in eyeglass prescription. In some cases, it can even lead to vision loss and the need for a cornea transplant.
In this article, we will explain what keratoconus is, what
causes it, how it is diagnosed, and what treatment options
are available. We will also share some interesting facts and
tips about living with keratoconus.
What is keratoconus?
Keratoconus is a condition where the cornea, the
clear front surface of the eye, becomes thin and bulges
outwards into a cone shape. The cornea is responsible for
refracting (bending) light rays that enter the eye and
focusing them on the retina, the light-sensitive tissue at
the back of the eye. When the cornea assumes an irregular
shape, the light rays are not focused properly, resulting in
blurry and distorted vision. Keratoconus may affect both
eyes, but usually not equally. One eye may have more severe
symptoms than the other. It generally begins to affect
people between their late teens and early 20s and progresses
over 10 to 20 years. The rate of progression varies from
person to person.
What causes keratoconus?
The exact cause of keratoconus is not well known,
although genetic and environmental factors are thought to be
involved. Around 10% of people with keratoconus also have a
parent with the condition. It is also more common in certain
populations, such as people with Down syndrome.
Some
possible risk factors for developing keratoconus include:
Eye allergies and eye rubbing, which can worsen the
condition.
Eye injuries or infections.
Chronic eye irritation or inflammation.
Exposure
to ultraviolet (UV) rays.
How is keratoconus diagnosed?
Keratoconus can be diagnosed by an ophthalmologist,
through a routine eye exam. The ophthalmologist may use
computerized corneal mapping to measure the shape and
curvature of the cornea. Corneal mapping can also measure
the thickness of the cornea, which is reduced in
keratoconus. This type of testing can often detect early
signs of keratoconus before the disease is visible.
Slit-lamp examination, a test that involves directing a
beam of light on the surface of the eye and using a
microscope to view the eye, is also employed for
diagnosing keratoconus.
Other tests
that may be done to diagnose keratoconus include:
Refraction, a test that uses special lenses and
equipment to measure your eyes and determine your
eyeglass prescription.
Keratometry, a test that involves focusing a circle
of light on the cornea and measuring the reflection.
This determines the basic shape of the
cornea.
Pachymetry, a test that measures
the thickness of the cornea using ultrasound
waves.
Improving vision with keratoconus
Improving vision depends on the severity of
keratoconus. Some of the vision correction options for
keratoconus include:
Special contact lenses. For more advanced cases,
special contact lenses, such as hybrid lenses, scleral
lenses, or piggyback lenses, may be prescribed. These
lenses provide better vision and comfort by creating a
smooth surface over the irregular cornea.
Corneal inserts. Another treatment option is
corneal inserts, also known as intacs. These are
small, curved devices that are surgically implanted
into the cornea to flatten and reshape it. Intacs
can improve vision and reduce the need for contact
lenses.
Corneal transplant. In some
cases, a corneal transplant may be necessary if the
vision loss is severe and cannot be corrected by
other means. A corneal transplant involves replacing
the damaged cornea with a healthy donor
cornea.
What are some tips for living with
keratoconus?
If you have keratoconus, here are some tips that can
help you cope with the condition and improve your eye
health:
Have regular eye exams and follow your
ophthalmologist’s recommendations for treatment and
care.
Avoid rubbing your eyes vigorously and avoid
allergens such as pollen and dust.
Wear sunglasses that block UV rays and protect
your eyes from dust and wind.
Use artificial tears or lubricating eye drops to
relieve dryness and irritation.
Clean and store your contact lenses properly and
replace them as instructed.
Seek
immediate medical attention if you experience any
signs of infection, inflammation, or rejection,
such as redness, pain, discharge, or decreased
vision.
Ayurvedic View on Keratoconus and Its
Management
In Ayurveda, there is no direct reference for
keratoconus, but based on the symptoms, it can be
considered as Timira, a Drshtigata Roga or disease
that affects the vision. Timira is further
classified into four types according to the
involvement of Doshas: Vataja, Pittaja, Kaphaja, and
Raktaja. Among these, vataja timira is the most
relevant for keratoconus, as it is characterized by
Vyaviddha Darsana (curved appearance of a straight
line), Avila Darshana (blurred vision or hazy
vision), Chandra, Deepadya Anekatvam (the luminous
objects like moon, lamp appear to be multiple), and
Kshina drushti (diminished vision).
According
to Ayurveda, the cause of timira is the vitiation of
both Vata Dosha, which is responsible for movement
in the body, and Alochaka pitta, the sub-type of
Pitta Dosha that governs vision. The factors that
can aggravate vata dosha and affect the alochaka
pitta are:
Ruksha Ahara (dry food),
Ati Laghu Ahara (light food), Vishama Ahara
(irregular food), Ati Tikshna Ahara (too spicy
food), Ati Katu Ahara (too pungent food), Ati Sita
Ahara (too cold food), Ati Ushna Ahara (too hot
food), Dushta Ahara (contaminated food), Adhyashana
(overeating), Viruddha Ahara (incompatible food),
Vishamashana (eating at improper time), Divaswapna
(sleeping during the day), Ratri Jagarana (night
awakening), Cinta (worry), Soka (grief), Krodha
(anger), Bhaya (fear), Ati Vyayama (excessive
exercise), Ati Abhyanga (excessive oil massage), Ati
Snana (excessive bathing), Ati Chakshushya Karma
(excessive eye strain), Dhumapana (smoking),
Madyapana (alcohol consumption), Anjana (eye
cosmetics), and Netra Abhighata (eye
injury).
These factors can lead to the weakening and
thinning of the cornea, resulting in the formation
of a cone-like shape. This causes the light rays
to be refracted irregularly, and impair the
vision.
The aim of ayurvedic management of keratoconus is
to balance both Vata Dosha and Alochaka Pitta, and
to strengthen and nourish the cornea. The general
principles of treatment are:
Nidana Parivarjana (avoidance of causative
factors)
Shodhana (purification therapy)
Shamana (palliative therapy)
Rasayana (rejuvenation therapy)
Chakshushya
(eye tonic) drugs
Nidana Parivarjana is the first and
foremost step in the treatment of any disease in
Ayurveda. It involves avoiding or minimizing the
factors that can aggravate Doshas and harm the
cornea. Some of the measures that can be taken
are:
Avoiding dry, light, irregular, spicy,
pungent, cold, hot, contaminated,
incompatible, or excessive food
Avoiding
daytime sleeping, night awakening, worry,
grief, anger, fear, excessive exercise,
excessive oil massage, excessive bathing,
excessive eye strain, smoking, alcohol
consumption, eye cosmetics, eye injury, and
eye diseases.
Shodhana is the process of eliminating
the accumulated toxins and impurities from the
body, and restoring the normal functioning of
the doshas and the tissues. Shodhana can be done
by various methods, such as vamana (emesis),
virechana (purgation), basti (enema), nasya
(nasal administration), and raktamokshana
(bloodletting). The choice of the method depends
on the condition and constitution of the
patient, and the advice of the ayurvedic
physician.
Shamana is the
process of pacifying the aggravated Doshas and
alleviating the symptoms of the disease. Shamana
can be done by various methods, such as Ahara
(diet), Vihara (lifestyle), and Aushadha
(medicine). The choice of the method depends on
the condition and constitution of the patient,
and the advice of the ayurvedic physician. For
keratoconus, the most suitable methods of Samana
are local ocular therapeutics, which include
Pindi, Bidalaka, Netra Prakshalana, and Tarpana.
These methods can directly act on the eye and
provide relief from the symptoms, as well as
prevent the progression of the disease.
Rasayana
is the process of rejuvenating the body and
mind, and enhancing immunity and vitality.
Rasayana can be done by various methods, such as
Ahara (diet), Vihara (lifestyle), and Aushadha
(medicine). The choice of the method depends on
the condition and constitution of the patient,
and the advice of the ayurvedic
physician.
Pathya or
compatible diet and lifestyle during and after
management of keratoconus includes the
following:
Eating fresh, wholesome, nourishing, and
balanced food at proper time and in proper
quantity
Following a regular and healthy daily
routine (dinacharya) and seasonal routine
(ritucharya)
Practicing eye hygiene and eye
care
Protecting the eyes from
dust, wind, sun, and other harmful
factors
Conclusion
Keratoconus is a challenging eye
condition that can affect the vision and the
quality of life of those who have it. Modern
medicine offers various treatment options to
correct the vision and slow the progression of
the disease, but they may have some
limitations, complications, or side effects.
Ayurveda, on the other hand, offers a holistic
and natural approach to manage keratoconus, by
balancing the vata dosha and alochaka pitta,
and strengthening and nourishing the cornea.
Ayurveda also emphasizes the importance of
avoiding the causative factors, following a
healthy diet and lifestyle, and taking
chakshushya (eye tonic) drugs to prevent and
treat keratoconus.
FAQ
Q : Can keratoconus lead
to vision loss or blindness, and are there any
complications associated with the
condition?
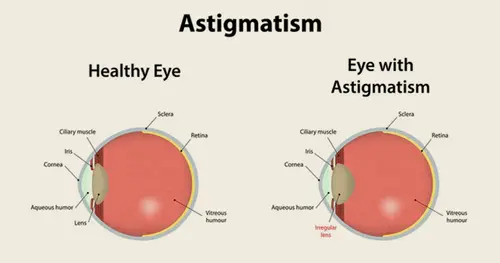
A : In
severe cases, keratoconus can lead to
significant vision loss or legal blindness,
particularly if left untreated. Complications
may include corneal scarring, hydrops (acute
corneal swelling), and irregular astigmatism,
which can severely impact visual
function.
Q : Is
keratoconus genetic?
A : In most
cases, keratoconus is not inherited
Q : Does Keratoconus Cause Eye Pain?
A : Keratoconus doesn’t always cause eye pain.
However, its symptoms can cause discomfort and
other problems. The most common symptoms of
Keratoconus include astigmatism, degrading
vision quality, and corneal thinning, bulging,
or rounding.
Q : Will
certain activities, such as sports or long
hours in front of the computer, hasten the
progression of keratoconus?
A:
There is no evidence that any physical or
visual activity has any effect on the
progression of keratoconus. The exception is
eye rubbing where the trauma caused by rubbing
the eye can damage the cornea which may cause
the condition to advance more
rapidly.
Q : Can
keratoconus affect my eligibility for certain
activities, such as driving or contact sports,
and are there any precautions I should
take?
A : Yes, keratoconus
can potentially affect eligibility for certain
activities, particularly those that require
good visual acuity and depth perception, such
as driving or contact sports. However, the
impact varies depending on the severity of the
condition .
Q : What is the
best contact lens for keratoconus?
A:
There is no single lens type or brand that
works for every keratoconus patient. In the
early stages, conventional soft lenses can
work remarkably well. As keratoconus
progresses, gas permeable (GP) lenses work
best for the majority of patients.
Q : Can laser eye surgery fix
keratoconus?
A : Keratoconus
is a degenerative disease that thins the
cornea and causes an abnormal shape, which
cannot be rectified with laser eye surgery.
Q :
Can Stage 3 keratoconus be cured?
A : Stage 3 is the most advanced. You will likely
have substantial corneal thinning and scarring
at this stage. We may use corneal ring
segments and corneal transplants (penetrating
keratoplasty) to treat the
keratoconus.

September 19, 2024
June 03, 2024
June 03, 2024
April 19, 2024
